Eligibility
-
Children 18 years old and younger,
-
Low-income adults ages 19-64 years old,
-
Citizen or qualified immigration status, and
-
Meet program income requirement
Get Help With Benefits
Our CFBU coordinators are available to assist families with enrolling and renewing public health benefits. To find your nearest coordinator, search for the name of your school or network below, or view our coordinator contact sheet. For more help, submit a Healthy CPS Assistance Request Form or call 773-553-KIDS (5437).
Enroll
Families enrolled in Medicaid will need to enroll in a Medicaid plan and should choose a primary healthcare provider that meets their needs. Medicaid Health plans include:
- Blue Cross Community Health Plans
- County Care Health Plan
- Meridian Health
- Molina Healthcare
- Aetna
For more information, reach out to your Children and Family Benefits Coordinator or call the Healthy CPS Hotline at 773-553-KIDS (5437) for assistance.
How To Use Your Medicaid Benefits
Once enrolled in Medicaid, CPS families have access to benefits that support their health and wellness. Completing the health risk screening and connecting to your Medicaid plan is essential to accessing health care services tailored to your needs and goals. Benefits include but are not limited to:
- Physician Services
- 24/7 Nurse Line
- Behavioral Health Services
- Lab Tests, X-Rays
- Hospital Services
- Vision and Dental Services
- Prescriptions
- Medical Supplies
- Transportation
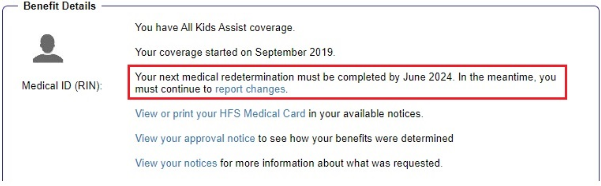
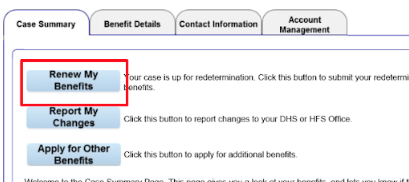
Medicaid Renewal
Since the Public Health Emergency ended, all families will need to start the Medicaid renewal process again, or they will lose their health insurance coverage.
If you or your family are enrolled in Medicaid, please follow the steps below to complete your renewal and ensure you remain enrolled in the program. Please keep in mind that Medicaid renewal dates vary by individual, and that a renewal must be completed every year.
If you need assistance with Medicaid renewal, you can call the Healthy CPS Hotline at 773-553-KIDS (5437) or fill out an assistance request form.